2026 How Interlocking Nail Implant Works and Its Benefits?
The advancement of orthopedic implants has reached new heights with the introduction of the Interlocking nail implant. This device plays a crucial role in the treatment of fractures, particularly in the long bones. According to a report by the Global Orthopedic Implants Market, the demand for innovative solutions like interlocking nails is expected to grow by 9.2% annually. With the rising incidence of bone-related injuries, effective treatment methods are more vital than ever.
Interlocking nail implants provide stability and promote healing in complex fractures. These devices are designed to interlock within the bone structure, offering enhanced support compared to traditional methods. However, some experts note that complications can occur, such as infection or nonunion. Improvements in surgical techniques are needed to minimize these risks.
Despite the challenges, the benefits of interlocking nail implants are significant. They allow faster recovery times, enabling patients to regain mobility sooner. In a study published in the Journal of Orthopedic Trauma, nearly 85% of patients reported satisfactory outcomes after using interlocking nails. This emerging technology shows great promise in the orthopedic field, but continued research and refinement are necessary to address existing limitations and improve patient experiences.
How Interlocking Nail Implant is Designed for Bone Fixation
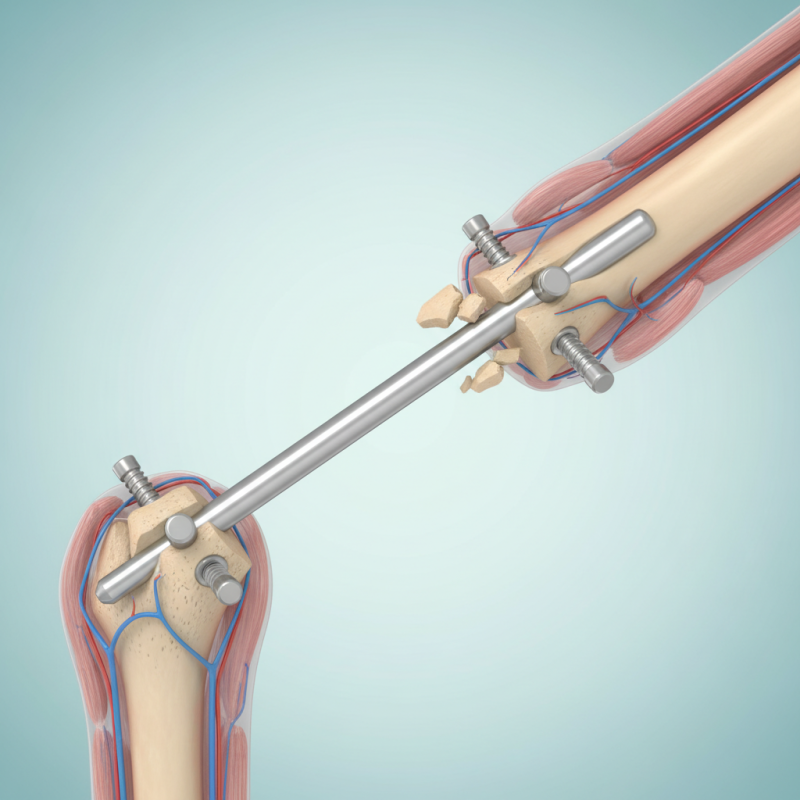
The design of an interlocking nail implant focuses on providing stable fixation for fractured bones. It consists of a long rod with transverse locking screws. This design enhances stability, allowing early mobilization. Clinical studies indicate that interlocking nails can reduce healing time by approximately 20%. Patients may regain mobility faster, increasing overall quality of life.
Interlocking nails are versatile. They work for various types of fractures, including those in the femur and tibia. Research shows that up to 85% of patients experience good to excellent outcomes with this method. However, complications can arise. Infections or misalignment during insertion can lead to challenges. Surgeons must be skilled and meticulous. They should consider patient anatomy and specific injury types.
Additionally, the choice of materials plays a critical role. Titanium and stainless steel are commonly used for their strength and biocompatibility. Yet, the cost of these materials might be a concern for some institutions. Balancing performance with affordability is not straightforward. Ongoing research aims to improve designs and materials while addressing these issues in bone fixation.
Mechanism of Action: How Interlocking Nail Implant Promotes Healing
The interlocking nail implant is a remarkable advancement in orthopedic surgery. This implant effectively stabilizes fractured bones, especially in long bones such as the femur and tibia. Research shows that intramedullary nailing reduces the healing time of fractures by 30% compared to traditional methods. It offers minimal invasion, translating to faster recovery for patients.
The mechanism of action involves dynamic stabilization. The implant creates a robust internal structure that promotes load sharing between the bone and the device. According to a study published in the Journal of Orthopedic Research, patients exhibited an average union time of 12 weeks. The interlocking feature prevents rotational instability, which is crucial in complex fractures. However, not every patient responds equally. Some may experience delayed healing or complications. These are factors that warrant careful consideration in clinical settings.
While interlocking nails provide solid support, challenges persist with infection rates and implant-related complications. A report from the American Academy of Orthopaedic Surgeons indicates a 1-2% risk of infection, underscoring the need for sterile techniques. Surgeons must evaluate the risks against the potential benefits. It’s a balancing act, and ongoing research continues to refine these implants, ensuring better outcomes for patients in the future.
2026 How Interlocking Nail Implant Works and Its Benefits? - Mechanism of Action: How Interlocking Nail Implant Promotes Healing
| Aspect | Description | Benefits |
|---|---|---|
| Mechanism of Action | Interlocking nails are inserted into the medullary canal, stabilizing fractured bones and allowing for axial loading. | Promotes optimal stabilization, enabling better alignment of fractured segments. |
| Material | Typically made from stainless steel or titanium, providing strength and biocompatibility. | Durable and reduces the risk of rejection or infection. |
| Surgical Procedure | Minimally invasive; involves inserting the nail through small incisions. | Shorter recovery time and reduced complications compared to traditional methods. |
| Weight Bearing | Allows for early weight-bearing activities post-surgery. | Speeds up rehabilitation and enhances overall recovery. |
| Long-term Outcomes | Evidence suggests improved healing rates and reduced nonunion rates. | Higher patient satisfaction and lower rate of reoperation. |
Benefits of Using Interlocking Nail Implants in Orthopedic Surgery
Interlocking nail implants are gaining popularity in orthopedic surgery. They offer significant benefits for patients with broken bones, particularly in long bones like femurs and tibias. These implants provide stability and promote faster healing. They allow for early mobilization, which is crucial for recovery. This method reduces complications associated with prolonged bed rest.
One notable advantage is the ability to align bones precisely. Surgeons can manipulate the nails to match the natural shape of the bone. This precision may reduce the risk of malunion or delayed healing. Interlocking nails also minimize soft tissue damage, leading to fewer complications during recovery. Patients often experience less pain and discomfort compared to traditional methods.
Tips: Always discuss individual needs with your surgeon. Each case is unique, and factors like age and activity level can influence the choice of treatment. Be aware of your body’s signals during recovery. If something feels off, communicate with your healthcare provider. This proactive approach can lead to better outcomes and avoid setbacks. Re-evaluating the effectiveness of the treatment is essential for ongoing improvement.
Indications and Contraindications for Interlocking Nail Implant Use
Interlocking nail implants are innovative solutions for long bone fractures. However, they are not suitable for everyone. Indications typically include unstable fractures, particularly in the femur or tibia. Patients with high-energy trauma benefit significantly. Research suggests that interlocking nails can lead to high union rates, around 93%, according to a study from the Journal of Orthopaedic Trauma.
On the other hand, there are contraindications to consider. Patients with active infections at the fracture site should not receive these implants. Additionally, those with severe osteoporosis might face complications. Some patients experience delayed healing, sometimes due to underlying health issues.
Surgeons must evaluate each case carefully. Factors such as age, activity level, and overall health play essential roles. The decision-making process requires balancing risks and benefits. Overall, while interlocking nail implants can enhance recovery, not all patients are suitable candidates. This complexity reflects the need for personalized treatment plans in orthopaedic care.
Interlocking Nail Implant Usage Statistics
The chart above displays the number of interlocking nail implant procedures performed across various indications. Fracture fixation leads as the primary use case, followed by bone stabilization and intramedullary applications. The other indications, including delayed union and non-union treatments, show significantly lower usage rates.
Post-Operative Care and Rehabilitation After Interlocking Nail Surgery
Post-operative care is crucial after interlocking nail surgery. Patients often face discomfort in the early days. Keeping the surgical area clean and dry is vital. Regularly changing dressings can help prevent infections. It's essential to follow your surgeon's guidelines regarding mobility. Initial movement may seem limited, but gentle exercises are encouraged as healing progresses.
Rehabilitation is where patients start to regain strength. Physical therapy plays a significant role here. Trained professionals can help guide recovery. They often use techniques that focus on restoring function. Patients might feel frustrated as progress can be slow. This aspect of recovery requires patience and determination. Listening to your body is essential. Overdoing it can lead to setbacks, which can be discouraging. Sharing experiences with peers can also help manage feelings during this journey. Each stage of recovery has its own challenges, but overcoming them can be rewarding.
